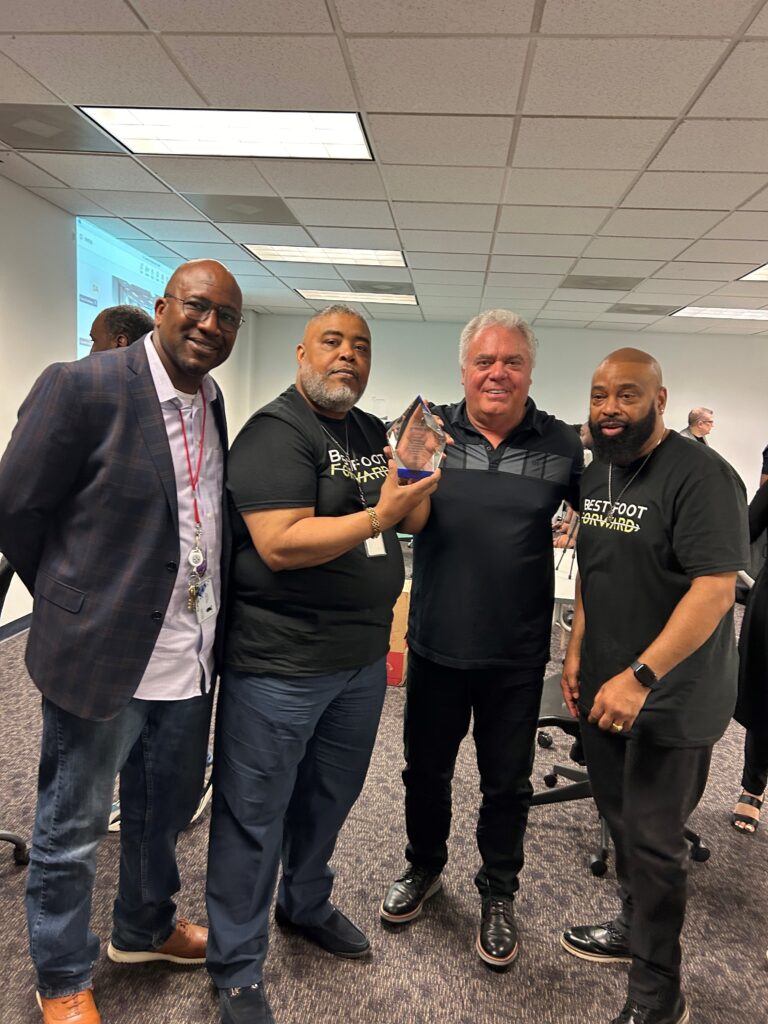
Celebrating Our Employees
It is with great pride and admiration that we come together to celebrate the remarkable achievements of our dedicated employees. Each milestone reached, each goal surpassed, is a testament to the talent, hard work, and unwavering commitment of our team. Congratulations to every member of our organization for your outstanding contributions and relentless pursuit of excellence. Your dedication fuels our success and inspires us all to reach greater heights. Thank you for your exceptional work and continued commitment to our shared vision. Here’s to many more milestones and successes together!